Delivery Complications
According to the Centers for Disease Control (CDC), delivery complications have surged in recent years due to increased maternal age, pre-existing chronic medical conditions, and pre-pregnancy obesity. Not only do delivery complications lead to increased medical costs and extended hospitalization stays, but they can negatively impact your health or that of your baby. Some problems stemming from complications accompanying the birthing process can be severe and even life-threatening.
Home > Delivery Complications
- Last Updated Date: March 24, 2025
To mitigate risks to you and your newborn, medical staff must carefully monitor you throughout your pregnancy and labor, and delivery and quickly intervene as needed. When obstetricians and other medical professionals fail to manage labor and delivery complications or pre-plan for potential problems, mothers and newborns can experience severe and sometimes permanent harm.
If you or your baby suffer injuries following negligent actions by your doctor or hospital or birthing center staff during delivery, it’s important to seek the help of a birth injury lawyer to investigate your case and evaluate whether you have legal recourse.
What causes complications at the time of delivery?
Labor and delivery often occur without significant problems. Severe complications are rare, and mostly, your doctor can anticipate and resolve any difficulties effectively. Other times, complications can develop unexpectedly or might be the result of negligence.
The probability of experiencing birth complications depends on your health history, current pregnancy, and the vigilance of your health care team. Additionally, different forms of delivery pose varying risks, including:
C-section delivery
Cesarean delivery is a birthing procedure in which a medical professional delivers a baby via an incision in the abdomen and uterus.
C-section is often necessitated by:
- Multiple gestations
- Prolonged or stalled labor
- Fetal distress or complications, such as hydrocephalus
- Newborn malpositioning
- Maternal infections, such as herpes or HIV
- An overly large baby
- Previous C-section delivery
- Maternal complications such as high blood pressure
- Uterine conditions such as uterine fibroids
- Placenta or umbilical cord anomalies
Delivery via C-section can also be a matter of maternal choice following:
- Fear of labor pains
- Anxiety about vaginal delivery
- Previous negative experiences or outcomes with vaginal deliveries
- The need for control over the delivery process
- Multiple social influences, including friends, family, and the media
- Interactions with medical professionals
No matter the reasoning for this surgical form of birth, a Cesarean delivery comes with risks of complications, including:
- Blood loss (up to 500mL more than vaginal delivery)
- Incision infection
- Blood clots
- Injuries to bowel, bladder, and other surrounding organs
- Adverse reaction to general anesthesia or medication
- Potential complications in future pregnancies
- Endometritis
C-section delivery can also result in breathing difficulties or surgical injury in newborns. Speak with a healthcare professional promptly if you suspect complications in yourself or your child.
Vaginal delivery
Vaginal delivery is the natural method of birth, pushing your baby through the birth canal. Your baby’s actual birth is the second stage of labor, typically lasting minutes to hours. The first stage of labor consists of uterine contractions, which lead to dilation of the cervix so that the baby can exit the mother’s body.
Even though vaginal delivery is common, with nearly 70% of U.S. births in 2017 happening via this delivery method, and typically the safest option for mothers and newborns, it is not without risks. Complications associated with the vaginal birthing process include:
- Tearing
- Postpartum hemorrhage
- Prolonged labor
- Maternal distress
- Injuries to the infant
- Incontinence in the mother
- Postpartum depression
- Intense anxiety in future pregnancies
Complications can worsen in labor induction, operative vaginal delivery, or when a doctor uses a vacuum extractor or forceps to deliver the baby. Operative vaginal delivery is associated with an increased risk for pelvic organ prolapse and fecal incontinence later in life.
Labor Complications and Severity
Differentiating between symptoms of normal labor and potential complications can be challenging, making it important for you to familiarize yourself with the most common delivery problems women experience so that you know when to alert your doctor for possible intervention. Your doctor should also closely monitor you and your baby throughout the labor and delivery process to detect any issues and offer prompt resolutions or emergency treatment when necessary.
Various labor and delivery complications include:
Different viral, bacterial, and parasitic infections can complicate labor and delivery, including:
- Urinary tract infections (UTIs)
- Cytomegalovirus (CMV)
- Bacterial vaginosis (BV)
- Group B Streptococcus (GBS)
- Influenza (flu)
- COVID-19 (coronavirus pandemic)
- Hepatitis B virus (can spread to the baby during birth)
- Yeast infections
- Zika virus (mosquito-borne illness)
These and other infections can be harmful to you and your baby. For example, in newborns, herpes can be life-threatening. It can also cause blindness, brain damage, and damage to other vital organs. In addition, bacterial vaginosis can play a role in preterm labor. It’s important to be proactive about seeking prompt treatment for any suspected infections during pregnancy.
The most common and safest position for a baby is with the head downward in the vaginal canal, and the face towards the mother’s back. However, not all babies descend this way. Some may be:
- Facing upward (also known as “sunny side up”)
- Lying sideways (horizontally across the uterus)
- In the breech presentation, either feet first (complete breech) or buttocks first (frank breech)
Depending on the baby’s position and other circumstances, medical professionals may:
- Use forceps to aid delivery
- Manually try to change the baby’s position
- Enlarge the vaginal opening
- Perform a Cesarean delivery
Overall, breech positions aren’t dangerous until delivery. During this time, the more complicated positions can increase the risk of cutting off the infant’s oxygen supply or the baby getting stuck in the birth canal.
Anemia occurs when the mother has fewer-than-normal red blood cells in her body. Its symptoms include:
- Pale or yellowish skin
- Breathlessness
- Irregular heart rate
- Frequent dizzy spells
- Chest pains
- Cold hands and feet
- Headaches
- Feeling weaker and more tired than usual
Anemia can be worse in case of hemorrhage or heavy bleeding during delivery, adding the risk of impaired cognition, fatigue, and depression. It also negatively affects mother-baby bonding. Folate deficiency anemia is especially dangerous in pregnant women and can lead to preterm labor and premature birth.
Gestational diabetes occurs when the mother cannot process sugars effectively, leading to higher amounts of glucose in the bloodstream. A diagnosis of gestational diabetes means the mother never previously had diabetes before pregnancy. However, it can affect multiple pregnancies, typically showing up mid-pregnancy.
Most women with this condition carry their babies to full term and deliver without complications with minimal diet and lifestyle changes. However, uncontrolled gestational diabetes can create problems after delivery. For example, a mother with gestational diabetes is at a higher risk of having a larger baby, necessitating a C-section or increasing the chance of birth injuries. Gestational diabetes can also result in breathing problems and hypoglycemia (low blood sugar) in newborns.
Placenta previa occurs when the placenta partially or fully covers the opening of the cervix. About one in 200 pregnant women will experience this complication. The most significant risk associated with this condition is severe bleeding as the cervix begins to dilate during labor. In some cases, the placenta will naturally migrate away from the cervix as the uterus grows. However, if the placenta is still covering the opening of the cervix at week 35 of pregnancy, then Cesarean delivery is usually performed.
Placenta previa is most common in women who:
- Smoke
- Have uterine fibroids
- Are 35 years and above
- Had four or more previous deliveries
- Have had in vitro fertilization (IVF) treatments
- Are pregnant with twins or other multiples
- Had previous uterine surgery, Cesarean delivery, or placenta previa
Usual symptoms include:
- Light to heavy vaginal bleeding
- Early contractions
- A large uterus size relative to the gestation of the pregnancy
- Breech presentation
Placenta previa can also increase the risk of developing placenta accreta, a life-threatening condition characterized by the placenta remaining inseparable from the uterine wall. Other threats to you and your baby include:
- Excessive blood loss (hemorrhage) and necessary transfusion
- ICU admission for you or your baby
- Need for a C-section
- Need for a hysterectomy after delivery if bleeding continues
- Premature delivery
- Low birth weight in your baby
- Lower APGAR scores in your baby (used to measure your baby’s heart rate, reflexes, muscle tone, breathing, and coloring)
- Respiratory distress or breathing complications in your baby, if delivered early
Low birth weight can result from poor nutrition, certain infections, or the use of drugs during pregnancy. Having a baby with a low birth weight increases the infant’s risk of:
- Blindness
- Heart infections
- Learning disabilities
- Respiratory infections
A baby born smaller than average may need to stay in the hospital’s neonatal intensive care unit (NICU) for up to several months after birth, especially if born prematurely.
Low birth weight isn’t always a complication or problem. Some babies born smaller than usual are perfectly healthy. Regular screening at routine prenatal visits to measure the fetus and identify potential risk factors can help mitigate possible health concerns.
High blood pressure happens due to the narrowing of the body’s arteries or blood vessels. It can be hereditary or caused by other lifestyle choices like smoking, sedentary behavior, or poor diet such as increased salt intake. If you suffer from high blood pressure before pregnancy, it can increase the risk of preeclampsia and preterm delivery. You also have a greater risk of giving birth to a small or underweight baby.
It’s important to work with your doctor to maintain your health and stabilize your blood pressure throughout your pregnancy.
Approximately 90% of women deliver within two weeks of their due date. However, in some instances, labor can start early (before the 37th week of gestation) or start late (after the 42nd week). Either scenario can endanger the baby’s health and life, which is why medical professionals need to monitor the baby’s progress and intervene when needed.
Preterm and post-term high-stress deliveries can result from pre-existing medical conditions or malpositioning of the fetus. Preterm labor occurs when labor pains start well before the 37th week of pregnancy, when the baby’s vital organs, like the brain and lungs, are not fully developed.
Preterm birth can lead to:
- Respiratory distress
- Jaundice
- Low birth weight
- Sepsis
- Vision problems
- Neurological injury
- Chronic lung disease
- Developmental delays
Premature babies must receive proper and immediate care to thrive.
Preeclampsia is common after the 20th week of pregnancy. It’s a condition characterized by high blood pressure and kidney or liver problems. It can be deadly for both the mother and her baby. The most effective treatment is delivery, but complications and recovery can sometimes persist even after the baby’s birth.
A miscarriage refers to the loss of pregnancy within the first 20 weeks, and it affects up to 20% of pregnancies among healthy mothers-to-be, according to American Pregnancy Association (APA).
A pregnancy loss after the 20th week is known as a stillbirth. It’s associated with:
- Infections
- Chronic maternal health issues
- Placenta anomalies
The miscarriage process often results in period-like cramps, only more painful. It can also cause heavy bleeding, including passing large blood clots or a recognizable fetus still in the pregnancy sac.
Fetal distress, recently renamed non-reassuring fetal status, describes a situation where the fetus is not doing well in response to pregnancy or labor.
Research links fetal distress to:
Low levels of amniotic fluids
Irregular baby’s heartbeat
Problems with muscle movement and tone
The condition can be caused by:
- Maternal anemia
- Insufficient oxygen levels
- Pregnancy-induced hypertension in the mother (preeclampsia)
- Meconium in the amniotic fluid
- Intrauterine growth retardation (IUGR)
Umbilical cords are prone to many difficulties. The cord may be too short or too long. It can also become compressed, knotted, or improperly connected to the placenta.
Umbilical cord problems can lead to delivery complications. For example, the cord might prolapse, coming out of the birth canal before the baby. It can also wrap around the baby’s neck, interrupting their breathing or descent.
Excessive bleeding can occur during delivery due to uterine tears, placenta previa, placental abruption, or the mother’s inability to deliver the placenta after giving birth to the baby. On average, women lose 500mL of blood during vaginal delivery and 1,000mL during a C-section delivery of a single baby.
Bleeding occurs 24 hours or up to 12 weeks after delivery. If the bleeding is severe, it can cause organ failure, low blood pressure, or even death. However, with proper medical care and prompt intervention, the outlook for both the mother and her baby is usually good.
Who's at risk of labor and delivery complications?
Women with the following medical conditions are at higher risk of having labor and delivery complications:
Cancer
Diabetes
High blood pressure

Epilepsy

Kidney problems

Anemia
Sexually transmitted infections (STIs) and other infections
Other factors that can increase the risk of complications during delivery include:
- Drinking alcohol
- Using illegal drugs
- Smoking cigarettes
- History of preterm birth
- Being 35 or older
- Young age
- Eating disorders like anorexia
- Carrying twins or triplets
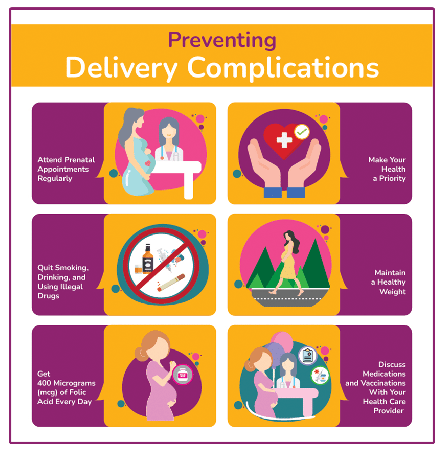
Preventing Delivery Complications
Some complications are unforeseen and thereby unpreventable, but the early detection and treatment of others can mitigate injury to both you and your baby. The following measures can help significantly reduce the risk of complications during labor and delivery:
Starting prenatal care as soon as you discover you’re pregnant is critical. Be sure to attend your prenatal care appointments regularly as scheduled, and reschedule any appointments that you have to miss.
OB-GYN visits, imaging appointments like ultrasounds, and blood and other screening tests allow your doctor to monitor your condition and that of your baby, keeping track of the baby’s growth, heartbeat, and overall health. These examinations also help identify and plan for possible pregnancy complications.
If you have a high-risk pregnancy, you should also keep your appointments with your maternal-fetal medicine specialist (obstetricians who specialize in high-risk pregnancies) as it increases the chances of early detection of problems and prompt determination of needed interventions.
Extreme fatigue, poor sleep patterns, high-stress levels, and poor diet contribute to labor and delivery complications. When pregnant, ensure that you get seven to eight hours of sleep as recommended. If you have difficulty sleeping at night because you’re uncomfortable, try to nap during the day when possible. Stick to a clean diet and healthy exercise regimen, and take measures to manage and lower your stress levels.
Also, avoid foods that may be harmful to the baby’s health, such as those that might contain listeria or salmonella. Common dangers are raw or uncooked eggs and lunch meat or cold cuts. Don’t consume unpasteurized cheese and milk, and wash vegetables and fruits thoroughly. In addition, cook meat thoroughly before consumption. Speak with your doctor or ask for a referral to a nutritionist if you need help maintaining a proper diet throughout your pregnancy, especially if morning sickness or food aversions are concerns.
Talk to your healthcare provider about controlling or treating pre-existing infections or medical conditions, especially those that can affect fetal development or cause birth injuries.
When you drink alcohol, smoke cigarettes, or use illegal drugs, these harmful substances either go directly to the fetus or cut off vital oxygen or nutrients, negatively affecting fetal development. Additionally, research links the use of illicit drugs to serious labor and delivery complications, such as preterm birth. Therefore, it’s best to cease using any recreational or non-prescription substances immediately after learning you’re pregnant.
Although quitting can be difficult, seeking support groups can be helpful. Your doctor can provide you with guidance and resources to help you make the healthiest choices for you and your baby. Reminding yourself of the complications and damage associated with these substances can possibly make the process easier.
Women with a pre-pregnancy BMI of 30 or more are at higher risk of developing labor and delivery complications and experiencing severe birth injuries.
If you’re overweight and want to get pregnant, talk with your physician about ways to get to a healthy weight. In addition, if you are underweight, you can meet with a dietician to make sure that you receive proper nutrition and learn what to eat to gain weight and better support the needs of a growing fetus.
Having enough folic acid in the body helps prevent significant brain and spinal damage in newborns. Get folic acid from fortified supplements or foods, and ingest the recommended amount per day. Speak with your doctor about your current folic acid levels and determine the amount you need to supplement daily.
Some prescription drugs can cause complications and birth injuries when taken during pregnancy. Still, a woman may need to use some of these medications to treat serious medical conditions. You should never stop or start taking any medications during pregnancy without discussing them with your doctor first.
Additionally, most vaccinations are safe and necessary to prevent illness like the flu, pneumonia, or COVID-19 during pregnancy. Nonetheless, it’s best to talk with your health care provider to ensure you get the right vaccines at the optimal time to keep you and your baby healthy
Different Treatment and Therapy Options
Treatment of complications that occur during pregnancy or during labor and delivery varies depending on the specific condition. Some common forms of treatment include:
- Rest
- Medications to ease labor pains and facilitate relaxation
- Use of birth-assistance tools if the fetus is already in the birth canal
- Oxytocin to provide stronger contractions
- C-section in case of maternal medical conditions and fetal distress
- Careful monitoring of iron levels
- Iron supplements and folic acid prescriptions
- Treatment of the underlying cause
- Changing the mother’s sleeping position
- Maintaining oxygenation for mothers
- Increasing maternal hydration
- Intravenous hypertonic dextrose
- Amnioinfusion
- Delivery by C-section
- Careful monitoring of the mother’s blood pressure
- Taking medications to keep the blood pressure under control
(This condition is extreme morning sickness that lasts throughout pregnancy, characterized by severe vomiting and nausea.)
- A diet of bland foods and plenty of fluids
- Medications
- Hospitalization if deemed necessary to acquire liquids via intravenous (IV) administration
- Delivering the baby if they are close to full term (between 37 and 40 weeks)
- Medication coupled with bed rest for cases happening earlier in pregnancy
- Use of forceps and other birth-assistance devices
- Episiotomy to surgically enlarge the vaginal opening
- Manually changing the fetus’s position
- Delivery by C-section
- Uterine massage
- Use of medication
- Uterine packing
- Removal of retained placenta
- Tying off bleeding arteries, veins, and capillaries
- Surgery to trace the cause of the excessive bleeding
- Hysterectomy in severe situations
- A healthy meal plan
- Mild to moderate daily exercise
- Insulin prescriptions
- Delivery by C-section
- Mechanical breathing or medications
- Providing oxygen to the pregnant woman
- Counseling
- Monitoring by medical professionals
- Giving your body time to heal
- Rest and reduced physical activities (for pregnancies under 20 weeks)
- Hospitalization in cases of heavy vaginal bleeding (followed by bed rest)
- Blood transfusions
- Early labor induction if the bleeding is uncontrollable
- C-section in case of preterm labor
- Bed rest in cases of minor separation
- Complete bed rest in cases of moderate separation
- Early delivery or immediate medical intervention for severe placental abruption
- Bed rest
- Medication to stop labor pains from progressing
- C-section in cases where delivery is unavoidable
- Rest
- Medications to ease labor pains and facilitate relaxation
- Use of birth-assistance tools if the fetus is already in the birth canal
- Oxytocin to provide stronger contractions
- C-section in case of maternal medical conditions and fetal distress
Written by:
Birth Injury Center Team
The Birth Injury Center aims to create informational web content and guides to help women and their families seeking support and guidance for birth injuries caused by medical negligence. All of the content published across The Birth Injury Center website has been thoroughly investigated and approved by medical expert Natalie Speer, RNC-OB, Attorney Ryan Mahoney.

