Intrauterine Fetal Demise (Stillbirth)
As the 5th leading cause of death worldwide, intrauterine fetal demise (IUFD), more commonly known as a stillbirth, is fetal death at the time of delivery. IUFD occurs when a fetus shows no signs of life, characterized as the absence or lack of breathing, heartbeat, and defined movements of muscles.
Home > Types of Birth Injuries > Intrauterine Fetal Demise (Stillbirth)
- Last Updated Date: November 22, 2023
The Centers for Disease Control and Prevention (CDC) recorded that fetal death occurs in roughly 1 in 100 pregnancies in the U.S. at 20 weeks of gestation or later and impacts roughly 1 in 160 births. There are three primary types of classification regarding stillbirth known as early, late, and term. IUFD is often misinterpreted or confused with miscarriages (happening before 20 weeks gestation) because both refer to the loss of pregnancy but differ based on when the loss occurs.
Causes of Intrauterine Fetal Demise
Possible causes of IUFD include:
When the baby remains in the womb for too long, the risk of fetal death increases. A post-term pregnancy, where the pregnancy continues to 42 weeks or more (dated from the last menstrual period), carries the highest risk, although the risk begins to increase after 40 weeks. The likelihood of this is higher during first-time pregnancies, but the risk is also increased in women who have experienced a previous post-term pregnancy.
Examples of maternal infections that can be dangerous to the fetus and possibly cause IUFD include certain sexually transmitted infections (STIs) such as HIV and syphilis and serious illnesses such as malaria. Infections can disrupt the growth of the fetus and increase the risk of preterm birth or lead to fetal death. Most frequently, maternal infections are a serious cause of organ damage and developmental delay.
Pregnant women with diabetes, obesity, high blood pressure, thyroid problems, or other chronic medical conditions are at a higher risk of experiencing intrauterine fetal death. Additionally, certain conditions that can be preexisting or develop during pregnancy can increase the risk. For example, women with preeclampsia, a condition that causes high blood pressure during pregnancy, have double the risk of placental abruption or stillbirth.
Fetal growth restriction (FGR) in pregnancy makes stillbirth seven times more likely to happen. Your doctor should regularly monitor and identify a small fetus before birth to create a plan of treatment that can help reduce the potential for IUFD from occurring.
While many deliveries happen safely, sometimes unexpected complications arise. Common complications during the birthing process that can lead to IUFD are kidney issues and breech positions. Sometimes, your doctor should be able to quickly identify these complications and adjust your birthing plan accordingly to mitigate risks to you and your baby.
The most well-known genetic abnormalities are cystic fibrosis, sickle cell disease, and Tay-Sachs disease. Gene mutations cause these inherited disorders that are similar to cytogenetic abnormalities in live births. A doctor can examine the fetus’s chromosomes if your pregnancy results in stillbirth using a karyotype test to discover if genetic abnormalities contributed to your loss.
The Rh factor is a protein that’s attached to red blood cells. Rh incompatibility means that a pregnant mother is Rh-negative, and a fetus’s blood is Rh-positive. If the baby’s blood and the mother’s blood mix (which is common during delivery), then her body will make antibodies against the Rh factor. In future pregnancies, these antibodies will travel through the placenta, attacking and destroying red blood cells in the fetus. This is known as Rh disease. Effects of Rh disease in a newborn include severe anemia, jaundice, brain damage, heart failure, and stillbirth. Rh disease can be prevented, which is why it’s very rare in women who have received appropriate prenatal care.
The placenta is a vital organ that forms in the lining of a woman’s uterus when she’s pregnant. It’s made up of both maternal and fetal tissue, and works with the umbilical cord to provide the fetus with nutrients and oxygen. If the placenta separates from the uterine wall before birth, this is called a placental abruption, and it deprives the fetus of the nutrients and oxygen that it needs. Placental abruption can also cause vaginal bleeding and mild to severe abdominal pain. Depending on how far along the mother’s pregnancy is, any issue with the placenta can potentially result in stillbirth without prompt medical intervention.
Stages of Intrauterine Fetal Demise
There’s no single timeframe during pregnancy that IUFD always happens. It can occur in the early, late, or term stages of pregnancy. No matter which trimester it happens, it never decreases or deters the severity of a parent’s emotional, mental, and physical response. Fetal demise is never an easy-to-read situation, and many times it’s confused with a miscarriage. All pregnancy losses are challenging, but there are some differences between them.
Miscarriage vs. Stillbirth
You should always contact your doctor if something feels or seems abnormal or you have questions about anything that concerns you. However, there are some signs and symptoms that might signal a problem with your pregnancy, including:

Early

Late
Fetal death that happens between weeks 28 and 36 of pregnancy is a late-term IUFD.

Term
Once a pregnancy reaches week 37 or more, it’s considered a completed or term pregnancy.
Navigate this Page

Has your infant suffered a birth injury as a result of malpractice or negligence? You may be eligible for compensation to cover treatment costs.

Signs and Symptoms of Intrauterine Fetal Demise
Many risks can accompany pregnancy, and with still so much being unknown behind the causes of intrauterine fetal demise, it can be easy to become concerned over the slightest things. That sense of urgency to check with your doctor and receive reassurance following proper testing and observation is a positive thing. It can potentially prevent complications and identify problems early on. However, it can also be overwhelming. So, often, it’s good to be aware and vigilant but not allow fearful outcomes to consume your thoughts during pregnancy.
Concerning IUFD, it can be confusing to know whether you’re at risk or when you should reach out to your doctor. It’s best to speak with your doctor about anything that you find concerning throughout your pregnancy. The signs and symptoms might not always present themselves the same for everyone, which is why it’s important to pay close attention and see your doctor if you fear something might be wrong.
What to Watch For During Your Pregnancy
You should always contact your doctor if something feels or seems abnormal or you have questions about anything that concerns you. However, there are some signs and symptoms that might signal a problem with your pregnancy, including:
- Monitoring movement: As the fetus grows and the child you’re carrying begins to develop, it’s common to feel movement throughout pregnancy. If you notice a lack of activity for many hours or days, you may be at high risk for IUFD.
- Spotting or bleeding: If this occurs during pregnancy, it could be a warning sign that something isn’t quite right, especially if the bleeding is excessive.
- Absent fetal heartbeat: This symptom can be diagnosed with an undetectable heartbeat following testing from a Doppler, stethoscope, or ultrasound.
- Sharp pains or cramping: Some slight cramps are normal when pregnant, but there might be a problem if they’re consistent and feel unbearable.
When to See Your Doctor
Aside from regular checkups, it can feel like you’re overreacting if you panic and call your doctor over every concern. The reality is that roughly one out of every 160 pregnancies in the U.S. results in stillbirth, which means that your concerns are valid. If at any given moment during your pregnancy you fear that something is wrong, it’s okay to call your doctor and get their professional advice or request that they run tests or perform scans to verify the safety and well-being of your growing child.
Should you start spotting or bleeding, experiencing abnormal cramping, notice a lack of movement, or find yourself feeling a high level of discomfort, You should visit your doctor as soon as possible. They’ll utilize a series of tests such as ultrasounds and use a stethoscope or Doppler to listen for the fetal heartbeat so that they can reassure you or determine if there’s a need for further action.
Intrauterine Fetal Demise Risk Factors
Your health is a priority when pregnant. However, many women may not be in the best health before or during their pregnancy. Certain conditions can increase the risk of intrauterine fetal demise.
Mother's Health Before and During Pregnancy
A history of pregnancy complications, obesity, hypertension, and many other medical issues can affect a mother’s health before and during pregnancy. Using prescription drugs for medical conditions such as high blood pressure, diabetes, and other conditions can also pose risks, but not controlling maternal illness could be worse.
Situational and environmental concerns such as alcohol, drug dependency, or domestic violence significantly impact a mother’s health before and throughout pregnancy. Exposure to alcohol, smoking, drug use, and physical abuse or chronic or extreme emotional stressors throughout the pregnancy can increase the risk of fetal death.
Race and Ethnicity
Unfortunately, women from some groups are more likely to experience IUFD than others. There’s a large gap between the number of fetal deaths experienced by African American women and white women. This is believed to be attributed to socioeconomic barriers and possibly genetic predispositions, although there’s not yet enough research to be sure about the cause of the disparity. In some situations, socioeconomic barriers prevent mothers from accessing prenatal care, leading to unrealized problems putting the mother and her baby at a greater risk for complications, potentially leading to a higher rate of fetal deaths.
Maternal Age
Domestic Violence
The mental and physical scarring from domestic violence (DV) can be traumatizing, affecting victims of all races, ethnicities, and ages. In communities with more significant socioeconomic barriers, there are more frequent associations between drug use and cases of domestic violence. When combined with pregnancy, the physical harm and emotional trauma from abuse can increase the risks of stillbirth.
Twins and Other Multiple Infant Pregnancies
Carrying more than one fetus can increase your chances of stillbirth. When women undergo in vitro fertilization (IVF), many specialists recommend transferring only one embryo per cycle into the uterus, to reduce the chances of premature birth and other potential complications. The more fetuses there are in the uterus at once, the higher the risk that one or more of them will experience intrauterine fetal demise.
History of High-Risk Pregnancies or Prior Stillbirths
Women who previously experienced a stillbirth or miscarriage are up to 10 times as likely to experience complications during future pregnancies. With a history of pregnancy complications such as fetal growth restriction (FGR) or preterm delivery, you’re likely at a higher risk of facing the same or new difficulties with subsequent pregnancies.
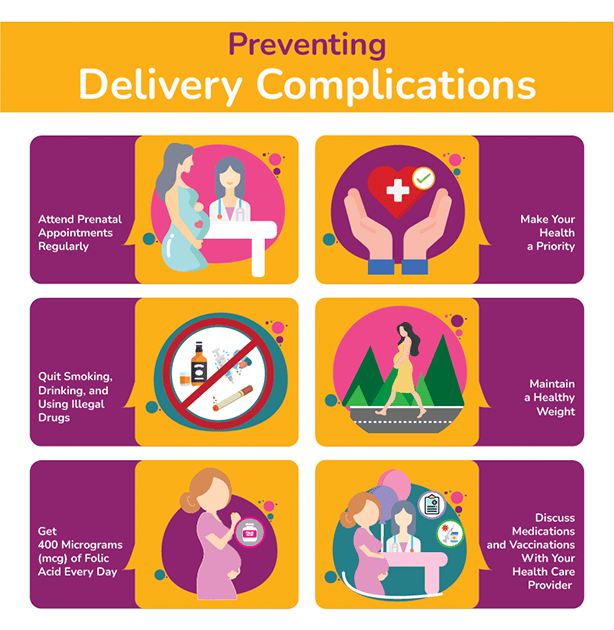
Preventing Intrauterine Fetal Demise
It’s important to understand that not all cases of IUFD are preventable. However, sometimes, it’s possible that you don’t have to suffer pregnancy loss with adequate and early intervention. It’s important that you attend all prenatal visits and that your doctor perform all routine monitoring or additional screenings necessary to ensure the safety of you and your unborn child.
If you miss an appointment, rescheduling it as soon as possible can allow your doctor to stay informed about your progress and determine if your care needs to be adjusted to cater to your current needs and those of your baby. Your prenatal visits are also excellent opportunities to ask questions and alert your doctor to any changes.
You cannot account for negligence by your doctor or health care team, but there are some additional preventative measures you can take to lower your pregnancy loss risks, including:
- Discontinuing smoking, drinking, or the use of any drugs that your physician has not prescribed, including over the counter or illegal drugs
- Sleeping on your side
- Staying active without overexerting yourself
- Trading less healthy foods for more nutrient-rich options
- Avoiding stressful situations to limit potential blood pressure increases and undue stress or anxiety
Diagnosing Intrauterine Fetal Demise

Doppler Ultrasound or Velocimetry: This checks for proper blood circulation in the fetus, uterus, and placenta.

Biophysical Ultrasound: Combined with a non-stress test, this checks vitals.

Ultrasound: A regular ultrasound checks for signs of movement and life.
Treating Intrauterine Fetal Demise
After receiving the diagnosis of stillbirth, processing the emotions of the loss is necessary throughout this devastating circumstance. Facing the loss of your unborn child is challenging, and while the pregnancy may be over, there are still medical procedures required to ensure your safety and recovery.
As a mother, understanding your options for removing the fetus is an important part of the process. In the past, many doctors performed dilatation and curettage (D&C) surgery to safely and properly remove the fetus and placenta.
Over the years, the options for removal have changed a bit, reducing the need for surgical procedures and replacing them with medications instead. Misoprostol and gemeprost are two commonly used medications, known as prostaglandin E1 (PGE1) analogs. They are used to bring about labor, to help safely deliver the stillborn fetus. If they wish, parents may be able to see and hold their stillborn baby afterwards, although this is entirely optional and is not possible in every case.
Risks of Not Removing a Fetus After Stillbirth
Hearing the news of your pregnancy loss can be overwhelming, and it can be tempting to want to avoid doing anything at all and simply be left alone to deal with your emotions. While spontaneous ejection is possible, it can also be extremely harmful and lead to severe blood loss or infections. Avoiding treatment can also cause damage to your cervix and uterus. It could be more detrimental to your health, even causing birthing complications later if you try to get pregnant again.
Coping with Intrauterine Fetal Demise
Losing a child is never easy. You’ll likely experience grief in the form of depression, anger, and anxiety. All of these emotions and feelings can exhaust you mentally and physically, harming your overall health. Grief following pregnancy loss from IUFD can leave you feeling unmotivated, lower your self-esteem, and even make you feel guilty about not being able to control the outcome. When this happens, it’s important to surround yourself with support to cope with your emotions and help yourself safely process your thoughts.
Your doctor may suggest seeing a therapist or prescribing temporary medications to assist in offering comfort as you work through this difficult time. You might consider reaching out to support groups to share your experiences with others who faced similar losses when you’re ready. You can choose between online or in-person group sessions at your own discretion and pace. Should you choose to utilize online resources, there are many public and private groups to choose from. You can also find local groups to join and share your experience.
It can be challenging to express how you’re feeling after your loss, and that’s completely normal. Allowing yourself time to grieve is important, but so is taking care of yourself. It’s okay to ask for help, even when it’s difficult, and you must remember you don’t have to walk through this tragedy alone.
