Erb’s Palsy
Home > Erb’s Palsy
- Last Updated Date: January 24, 2025
What is Erb's Palsy?
Erb’s palsy, also known as Erb-Duchenne palsy or brachial plexus palsy, is a type of injury to certain nerves of the arms. It most commonly occurs during birth, although the injury can also occur during the first few months of life. Erb’s palsy is caused by traumatic force that damages the baby’s brachial plexus, a critical network of nerves near the neck. These nerves originate from the spinal cord, and are responsible for both feeling and movements in the fingers, hand, and arm.
The brachial plexus consists of several large nerves, which transport electrical signals back and forth between the brain and the arm and hand. Injury to the nerves interrupts this communication. This results in loss of motor function, which causes the arm to be underdeveloped, weak, and in some cases paralyzed. It can also cause loss of sensory function, which results in areas of numbness.
Erb’s palsy specifically involves damage to the nerves in the upper part of the brachial plexus. This is the most common form of brachial plexus birth injury; because of the anatomy of the area, these nerves are the most vulnerable to damage. If the baby has damage to both the upper and lower nerves, then this is known as a global brachial plexus birth palsy.

Types of Erb's Palsy
Studies reveal that 2 in every 1,000 children suffer from Erb’s palsy. The debilitating condition is often the result of the nerve fibers of the brachial plexus undergoing stretching due to the baby’s shoulder and head moving in different directions, commonly seen in difficult deliveries.
Erb’s palsy falls under four primary classifications, including:
Avulsions
In an avulsion, the nerve has torn away from the spinal cord, causing severe motor impairment. Avulsions generally don’t heal on their own, but various treatments, including surgical interventions, are effective in helping babies regain mobility. Many children continue to have some lifelong challenges related to the injury, but are able to function well.
Rupture
A rupture occurs when a nerve is completely torn, but not at the level of the spinal cord. Like avulsions, ruptures generally don’t heal on their own. A surgical procedure can help to regain some mobility. This is often a nerve transfer or nerve graft procedure, which uses healthy nerves to replace the damaged ones, helping the affected area to resume feeling and some level of mobility. Many children still have some lifelong effects from their condition, but often recover a good level of function.
Neuroma
This form of Erb’s palsy injury occurs when nerves are damaged, resulting in scar tissue formation. The scarring presses on the healthy nerves and causes discomfort characterized by a burning sensation. Treatment for a neuroma includes surgery and physical therapy. In some cases, your child may experience a full recovery.
Neuropraxia
This is the mildest type of Erb’s palsy, and is caused when the nerve fibers are stretched but not torn. Neuropraxia is the most common and easiest form of Erb’s palsy to treat. In most cases, your baby should fully recover in three months. However, some instances result in severe discomfort and burning pains during the recovery period.
Signs of Erb's Palsy
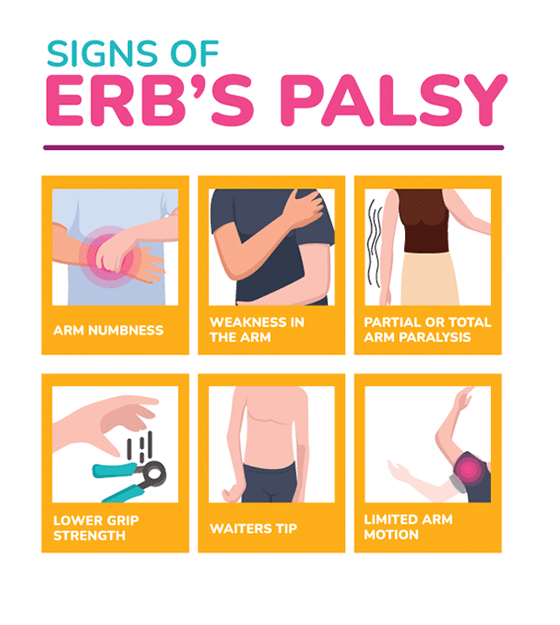
The signs and symptoms of Erb’s palsy vary based on the specifics of your child’s injury. Some of the possible signs include:
- Arm numbness
- Weakness in the arm
- Partial or total arm paralysis
- Low grip strength
- Waiter’s tip (when the wrists rotate inwards and the arms simply hang by the side)
- Limited arm motion
Common Causes of Erb’s Palsy
Erb’s palsy is relatively rare. It causes significant arm weakness in up to 5 of every 10,000 births. The main risk factors for developing the condition include:
Improper use of birthing tools during delivery
If medical professionals pull the baby forcibly and quickly from the birth canal, this can cause neck and shoulder injuries. Improper or excessively forceful use of tools like forceps and vacuum extractors can lead to Erb’s palsy.
Gestational diabetes
Babies born to mothers with gestational diabetes often have a high birth weight. This leads to a more difficult delivery, creating an increased risk for Erb’s palsy and other birth injuries. Doctors should screen for, monitor, diagnose, and treat gestational diabetes in order to minimize this risk.
Breech birth or other abnormal position
The ideal position for the baby at the time of delivery is head down, face towards the mother’s back. A Breech birth occurs when the baby is in a feet-first or bottom-first position. This increases the risk of Erb’s palsy, as the baby’s shoulders and arms are more vulnerable to injury in this position and the labor tends to be longer and more difficult. Other abnormal positions, such as head down but face forwards, can also increase the risk by making labor longer and more challenging.
Prolonged labor
The second stage of labor, also known as the “pushing stage,” begins when the cervix is completely opened, and ends when the baby is delivered. Long or difficult labors increase the amount of time that the baby spends in the birth canal and can put excess pressure on the baby, which increases the risk of injury. In addition, medical professionals may need to intervene and use tools to assist in delivery, which creates an additional risk of injury.
Large baby
A larger baby (with greater birth weight or length) increases the risk of brachial plexus injuries during delivery by increasing the risk of a long or difficult labor. Although gestational diabetes is the most common reason for a baby to have a high birth weight, other factors can also lead to this, including a late (postterm) delivery, excessive maternal weight gain, and genetics. If the mother’s body is small, the birth canal may be small relative to the baby, which also increases the risk of a long or difficult labor.
When to See Your Child's Pediatrician About Possible Erb's Palsy
In most cases, the symptoms of Erb’s palsy will be recognizable soon after birth. However, it can be difficult to determine the full extent of nerve damage until the baby is about three to six months old.
If your child starts showing any of the possible symptoms of Erb’s palsy within three months after delivery, it’s a good idea to discuss this with your child’s pediatrician. Doctors may conduct certain tests to assess the possible nerve damage.
Diagnosis of Erb's Palsy
To determine whether your baby has Erb’s palsy, the first step is for your physician to conduct a thorough physical examination. The doctor will evaluate the baby’s arm function, including their muscle strength, range of motion, and ability to feel touches on the arm. If the exam indicates a problem, then the next step is to use testing to evaluate the function of the muscles and nerves of the arm, as well as to look for the location of damage within the nervous system. This will allow the doctor to pinpoint your child’s diagnosis. The following tests are generally performed:

EMG
EMG, or electromyography, is used to assess the function of muscles. This test involves stimulating muscles with gentle electrical impulses, and measuring their response.

Nerve Conduction Studies
This test is used to measure the ability of nerves to conduct electrical impulses. Doctors will measure how fast an electrical impulse flows from one part of a nerve to another. Together with the EMG, these tests allow doctors to determine whether muscle damage or nerve damage is the cause of your child’s weakness.

Imaging Studies
Common imaging tests used to diagnose Erb’s palsy include ultrasounds, X-rays, CT scans, and MRIs to help identify nerve damage between the neck and shoulder. Sometimes, your child’s pediatrician might also order laboratory tests.
Treatment for Erb’s Palsy in Your Newborn
In mild cases of Erb’s palsy in newborns, the condition can resolve on its own within a couple of months. However, severe cases require medical intervention, especially if your child’s development and range of motion is still limited after they’re past the six-month mark.
Erb’s palsy treatment options include both non-surgical and surgical interventions, such as:
Non-Surgical Treatments
In mild cases of Erb’s palsy in newborns, the condition can resolve on its own within a couple of months. However, severe cases require medical intervention, especially if your child’s development and range of motion is still limited after they’re past the six-month mark.
Erb’s palsy treatment options include both non-surgical and surgical interventions, such as:

Physical Therapy
In mild cases of Erb’s palsy in newborns, the condition can resolve on its own within a couple of months. However, severe cases require medical intervention, especially if your child’s development and range of motion is still limited after they’re past the six-month mark.
Erb’s palsy treatment options include both non-surgical and surgical interventions, such as:

Occupational Therapy
An occupational therapist uses various movement exercises to improve your child’s muscle tone and enhance joint function. Occupational therapy focuses on learning to perform daily tasks in the most efficient way, as well as on regaining functional sensation in the affected arm. For a baby, the tasks might include things like holding bottles and picking up toys. Babies with Erb’s palsy may start occupational therapy within a few days of birth.
Physical and occupational therapies help prevent joint contracture, where the joints become permanently stiff, by maintaining a reasonable range of motion in the hand, wrist, elbow, and shoulder. However, non-surgical treatment options should happen regularly for the best results. Parents should take an active role in helping their children keep their joints and muscles fit since babies can’t do so alone.
Surgical Treatments
If your child doesn’t show significant improvement from physical and occupational therapies after three to six months, your child’s physician might suggest surgery. In some cases, a surgical procedure can help to restore some of the lost motor and sensory function in the arm and hand. Microsurgery, an advanced technique which uses a high-powered microscope to allow the surgeon to accomplish very delicate tissue repairs, has been used to accomplish good outcomes for many patients. Surgical options for Erb’s palsy include:
Nerve transfers
The surgeon disconnects part of a nerve from another muscle and reroutes it to the muscles that have been affected by Erb’s palsy.
Nerve grafts
The surgeon takes a piece of a healthy nerve from another part of the body and uses it to replace a section that was damaged by Erb’s palsy. In a nerve transfer, only one end of a nerve is moved, while the other end is left in place; in a nerve graft, an entire piece of a nerve is removed from one place and put somewhere else.
Tendon transfer
This procedure involves moving a tendon and part of a muscle from one location to another, in order to restore the ability to perform certain important movements.
Releasing joint contractures
A joint contracture occurs when the connective tissue around a joint becomes thick and stiff, restricting its range of motion. This is common when a joint is immobilized for a long period of time. Cutting the thickened tissue can release the joint and improve its range of motion.
Nerves heal slowly and often take months or sometimes years to fully recover. It will be important to be diligent about your child’s rehabilitation exercises in order to maximize the benefit of surgery. Other types of therapy may also be used in order to help the child regain strength and range of motion.
Although therapy and surgery often improve a patient’s symptoms, many children with Erb’s palsy continue to experience some symptoms even after treatment. In some cases, the condition will improve over time, but this doesn’t always happen. Your child’s doctor will continue to monitor their progress, and may recommend additional surgery in the future if this is warranted.
Preventing Erb’s Palsy in Newborns
In most cases, Erb’s palsy is preventable in two main ways:
High-quality maternal health care
Excellent health care is especially important in pregnant women with gestational diabetes, ensuring their blood sugar is well regulated, reducing the infant’s chances of being larger and sustaining brachial plexus or head or neck injuries during birth. Close monitoring of the mother and baby can ensure your health care team becomes aware of any problems early and takes appropriate actions to mitigate risks.
Advanced planning
If your doctor notices the fetus is in an incorrect birthing position during late pregnancy or is larger or smaller than normal, especially in the weeks leading to delivery, your obstetrician can devise treatment plans and inform you of your options for your and your child’s optimal safety and well-being. Your health care team can ensure that your birthing plan is adequate for your specific circumstances and have alternate plans in place with skilled staff members available in case of complications. In some cases, Cesarean delivery or an induction of labor may be the safest option for your baby.
Resources for Parents Dealing With Erb's Palsy
If your child suffers from Erb’s palsy due to birthing complications, connecting with other parents facing the same challenges can make a significant difference and provide you with much-needed emotional support. Joining support groups also equips you with new insights, additional information, possible treatment recommendations, and advice to help you better manage your child’s condition.
You should always speak with your pediatrician about any changes to your child’s health care, but it’s helpful to do your research so that you can ask your child’s doctor questions to determine the best possible course of treatment.
National organizations that provide Erb’s palsy resources and information about support groups include:
- The Birth Trauma Association
- Mothers United for Moral Support
- Brachial Plexus Palsy Foundation
- United Brachial Plexus Network
You can also consider joining social media groups online and local support groups in your community. Your child’s doctor might be able to point you in the right direction for guidance.
Seeking Medical Help and Legal Action for
Your Infant's Erb's Palsy Diagnosis
If you notice signs and symptoms of Erb’s palsy in your infant, including arm numbness, weakness or paralysis, limited arm motion, or waiter’s tip, you should bring this to the attention of your child’s doctor.
If you suspect a doctor’s or other health care provider’s negligence or wrongdoing before or during birth caused your child’s Erb’s palsy diagnosis, you should seek legal help. You may be eligible to file a birth injury lawsuit for financial compensation, which can help you pay for medical bills and treatment for the care of your child.
Written by:
Birth Injury Center Team
The Birth Injury Center aims to create informational web content and guides to help women and their families seeking support and guidance for birth injuries caused by medical negligence. All of the content published across The Birth Injury Center website has been thoroughly investigated and approved by medical expert Natalie Speer, RNC-OB, Attorney Ryan Mahoney.
