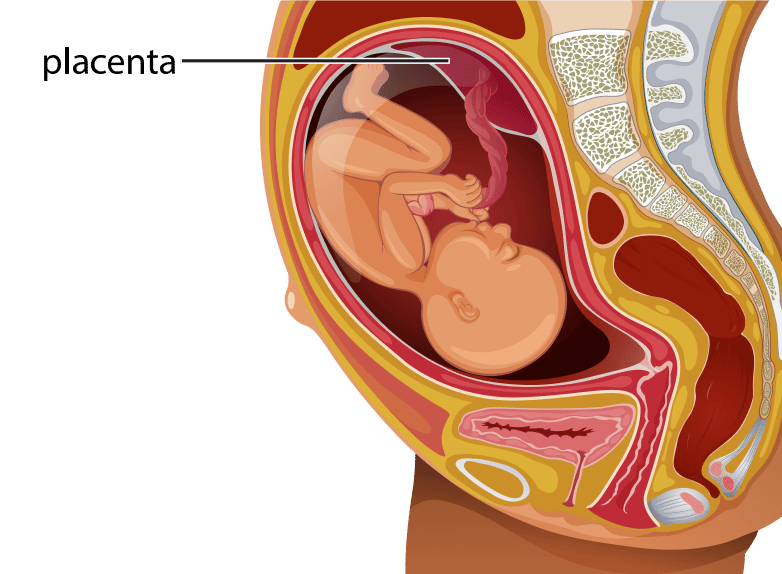
Placenta Previa
Placenta previa is a condition that occurs when the baby’s placenta partially or totally covers the mother’s cervix.
It occurs in about 1 out of every 200 pregnancies, according to the March of Dimes. If placenta previa occurs early in the pregnancy, it will often resolve itself; however, it can result in severe complications if it occurs later in the pregnancy. Placenta previa during labor and delivery can put mother and baby at risk.
Home > Pregnancy Complications > Placenta Previa
- Last Updated Date: January 27, 2025
Placenta previa has three types, according to the American Pregnancy Association:
- Complete placenta previa - The cervix is completely covered by the placenta.
- Partial placenta previa - A portion of the cervix is covered.
- Marginal placenta previa - The position of the placenta causes it to extend just to the edge of the cervix.
What causes placenta previa?
- In vitro fertilization
- Cigarette smoking
- Cocaine use
- Previous Cesarean delivery
- Age (35 years old or older)
- Previously pregnancy
- Multiple fetuses
- History of placenta previa
- Reproductive surgery (e.g., myomectomy or dilation and curettage)
Placenta Previa Symptoms
- The baby is breech.
- The uterus measures longer than it should.
- The pregnant woman is experiencing premature contractions.
How is placenta previa diagnosed?

What is the treatment for placenta previa?
What are the possible complications?
Preterm Birth
The mother may experience severe bleeding during the pregnancy. In this case, the doctor may have to schedule an emergency Cesarean delivery before 34 weeks of pregnancy. The premature baby is at greater risk for breathing issues and birth injuries such as cerebral palsy and hypoxic-ischemic encephalopathy.
Hemorrhage
Life-threatening bleeding can occur during labor, delivery, and post-delivery. Postpartum hemorrhages cause 12 percent of maternal deaths in the United States, according to American Family Physician. Doctors often prescribe medication or transfusions to treat hemorrhages.
Placenta Accreta
Placenta previa increases the risk of placenta accreta. Placenta accreta occurs when the placenta grows into the uterine wall. Instead of detaching from the uterine wall after childbirth, all or part of the placenta remains attached.
Placenta accreta also can cause severe blood loss. To control this severe bleeding, the patient might require a hysterectomy — full removal of the uterus. Placenta accreta can also require preterm delivery, leading to complications such as fetal hypoxia, another effect of oxygen deprivation. Fetal hypoxia can result in significant issues of brain and neurological function, according to Frontiers in Neuroscience.
Placental Abruption
Placental abruption occurs when the placenta “partly or completely separates from the inner wall of the uterus before delivery,” according to the Mayo Clinic. It also can decrease or block the baby’s supply of oxygen and cause heavy bleeding for the mother. Placental abruption is more likely in cases of placenta previa.
Preventable Causes of Birth Injuries Associated with Placenta Previa
- Failure to order an ultrasound
- Attempting a vaginal delivery
- Failure to continuously monitor the baby's health
- Performing a pelvic exam
- Failing to perform a timely Cesarean delivery
Seek Help
We at Birth Injury Center understand the challenges of life without a partner or with a special needs child. If you think medical malpractice may have caused injury to you or your baby, contact us today.

Written by:
Birth Injury Center Team
The Birth Injury Center aims to create informational web content and guides to help women and their families seeking support and guidance for birth injuries caused by medical negligence. All of the content published across The Birth Injury Center website has been thoroughly investigated and approved by medical expert Natalie Speer, RNC-OB, Attorney Ryan Mahoney.


