NEC Treatment
Necrotizing enterocolitis (NEC) affects the tissues of a baby’s intestinal wall. It can cause a hole to develop in the intestine, allowing material from inside the intestines to spill into the abdomen. This disease occurs most often in premature babies, who are much more likely to contract the illness than full-term infants. Approximately one in 1,000 premature babies develops NEC.
Home > Necrotizing Enterocolitis (NEC) > NEC Treatment
- Last Updated Date: September 15, 2023
Risk factors for NEC include low birth weight and premature birth. Formula feeding, rather than feeding with human milk, may also increase the risk. Signs of NEC include bloody stool, diarrhea, lethargy, and green or yellow vomit. An infant may refuse to eat or fail to gain weight. Early treatment of NEC is essential for saving as much intestinal tissue as possible.
NEC treatment options range from simple to complex, and severe cases may require surgery. Advanced cases may result in lifelong complications. During treatment, babies may need to stay in the neonatal intensive care unit (NICU).
Treatment options for this potentially deadly gastrointestinal disease include the following:
- Antibiotics
- Catheters
- Isolation
- Nasogastric tubes
- Oxygen or breathing machines
- Surgery
Early diagnosis of NEC can help to prevent significant complications. The infant may receive intravenous feeding, rather than feeding by mouth, to allow the bowels to rest and repair. In the most severe cases, doctors may need to perform multiple surgeries within the abdominal cavity over the course of several weeks.
NEC has an 80 percent survival rate when the disease is caught early enough for the infant to receive treatment. Doctors should closely monitor an infant’s heart rate; by looking for abnormal heart rate patterns, they may be able to find a serious problem early, such as NEC or sepsis (an infection in the bloodstream).

Antibiotics
Common antibiotics used during treatment of NEC include gentamicin and ampicillin, which may be combined with metronidazole. Antibiotic treatment will usually last 10 to 14 days.
Some infants may recover after receiving antibiotics without any need for further treatment. The bowels and intestinal wall can heal in mild cases of NEC, particularly when only a portion of the bowels is affected.
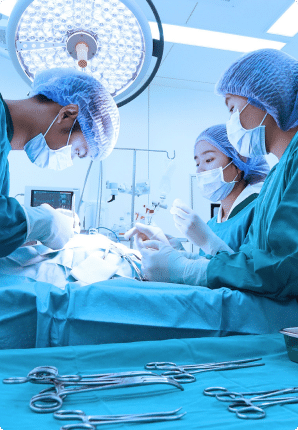
Surgery
Approximately one-fourth of infants diagnosed with NEC must undergo surgical intervention. The goal of surgery is to remove dead and dying intestinal tissue, while saving as much tissue as possible.
Surgical treatment for NEC requires general anesthesia and a laparotomy, or an incision through the wall of the abdomen. The surgeon removes dead bowel tissue and attempts to reconnect the healthy ends of the remaining intestinal tissue. After surgery, an infant may temporarily have an ostomy; this is an opening through the abdominal
wall for waste to leave the body. Ostomies are needed when some parts of the bowel are not healthy enough to reconnect right away. This diverts waste and gives the bowel tissue time to rest and heal. Usually, the baby will return after a few months for another surgery to reconnect the intestines, and the ostomy will be removed.
Over the long term, infants who have had surgery for NEC may experience a condition called short bowel syndrome or short gut syndrome. This occurs when the infant doesn’t have enough tissue left in the small intestine to absorb adequate nutrients.

Peritoneal drainage
Some babies are too premature or too small to undergo surgery. As an intermediate step, doctors may place a drain through the abdominal wall. This allows air, fluid, and pus to drain from the abdomen. A surgical procedure can be performed later if needed.
Studies have indicated that drain placement is an effective treatment modality for NEC, and some research suggests that it may be beneficial to try using a drain first even on NEC patients who are eligible for surgery.

Isolation
Preterm infants who encounter infection-causing bacteria may be at risk for contracting other diseases during NEC treatment. Doctors have reported a variety of fungal, viral and bacterial infections occurring alongside diagnoses of NEC. Premature infants may be kept in isolation during therapy, to reduce the child’s chance of contracting an additional infection.
Nasogastric Tube
A nasogastric tube or oral-gastric tube carries food and medicine directly to an infant’s stomach. Also known as enteral nutrition or enteral feeds, the nasogastric tube will deliver the protein, fat, carbohydrates, minerals and electrolytes the infant needs to survive. The tube also drains air and fluid from the stomach and prevents material from reaching the bowels. The infant may have a nasogastric tube for up to 10 days while in a children’s hospital or specialized unit during the course of antibiotics.
Some infant patients may require parenteral nutrition, which is where nutrients aren’t delivered to the stomach and are instead delivered intravenously. Parenteral nutrition is often used when an infant develops short bowel syndrome, leaving them unable to efficiently absorb nutrients through the digestive system.

Supplemental Oxygen or a Ventilator
Infants with NEC may have severe abdominal swelling, which can create difficulty breathing. Health care providers may administer oxygen through a facial tube, or even place the infant on a breathing machine to help ensure that they get enough oxygen.
Recovering from NEC and Further Treatment
Infants who recover from NEC may require further treatment or observation as they grow. Some children develop a condition known as intestinal stricture, which occurs when the diameter of the intestines shrinks due to scar tissue, making it difficult for food to pass through during digestion. Infants may require further surgeries if they develop strictures.
In some cases, children who survive and recover from NEC may not get enough nutrients to grow because of a reduction in their ability to absorb those nutrients. Sustained nutrient deficiencies may result in developmental delays. Some specialized treatments may become necessary to boost nutrition in infants and children recovering from NEC.
Please contact us to learn more about your options after a diagnosis of necrotizing enterocolitis. The Birth Injury Center is here to support you.
Written by:
Birth Injury Center Team
The Birth Injury Center aims to create informational web content and guides to help women and their families seeking support and guidance for birth injuries caused by medical negligence. All of the content published across The Birth Injury Center website has been thoroughly investigated and approved by medical expert Natalie Speer, RNC-OB.

