Brachial Plexus Injuries in Newborns
Home > Brachial Plexus Injuries in Newborns
- Last Updated Date: December 6, 2023
What is a brachial plexus birth injury?
The brachial plexus is a network of nerves that allows us to move our hands, arms, and wrists. These nerves also give us the ability to lift our arms, control muscles in our chest, and receive sensory input in our upper limbs. The nerves of the brachial plexus originate from the spinal cord at the level of the neck. They come together in the upper chest and armpit to form the brachial plexus. From the brachial plexus, the five main nerves of the arm emerge.
Sadly for parents and their children, injuries can happen to infants’ brachial plexus during birth. Brachial plexus injury occurs in about one to three out of every 1,000 births. Tearing, stretching, or compressing their tiny nerve system during difficult deliveries can create communication problems between the spinal cord and their arms, hands, and wrists. Loss of muscle function or even upper-arm paralysis can result from an injury to the brachial plexus.
Types of Brachial Plexus Injuries
There are numerous different brachial plexus injuries that can potentially lead to an array of resulting medical conditions. Injury types and severity depend on how the nerves are damaged and the extent of their injury.
One terrible result can be Erb’s palsy, where the baby’s nerves in the neck are so damaged that its arms are partially or fully paralyzed. Klumpke’s palsy, another serious brachial plexus injury suffered at birth, typically affects the forearm and hand. Avulsion injuries (also known as Horner’s syndrome) are associated with nerve injury that causes a child to have drooping eyelids, smaller eye pupils, and sometimes limited sweat production in their face.
Let’s look at three of the most common brachial plexus injury categories:
Stretched
Stretching of the nerves is the most common and mildest brachial plexus injury. With this injury, the nerves are stretched but not torn. Most babies’ nerves heal on their own from a stretching injury within their first three months. The technical name for this stretching injury is Brachial Plexus Neuropraxia. It’s usually caused by compression or traction of the nerve.
Ruptured
The next category of injuries is ruptures — another common type of brachial plexus injury that is more serious than stretching. A rupture happens when a nerve is torn, but not at the site of its attachment to the spinal cord. A very forceful stretch can partially or completely tear the nerve.
Nerve ruptures can weaken the shoulder, arm, or hand muscles. Certain muscles can become unusable with this injury, and ruptured brachial plexus nerves may need surgical repair. Nerve rupture can be very painful and is considered a more serious injury than neuropraxia (a stretching injury that does not tear the nerve).

Avulsion
When a nerve root is torn from the spinal cord, it is called an avulsion. This category of brachial plexus injury is less common than stretch and rupture injuries, occurring only in 10% to 20% of cases. Surgical repair is complicated as nerve tissue from another area must be surgically transferred to replace the nerve torn from the spinal cord.
Signs and Symptoms of Brachial Plexus Injuries
How do you know if your baby has a brachial plexus injury? First, watch for any indication that they are having trouble moving their arm or hand. Also, a limp or oddly positioned arm can be a sign of brachial plexus injury. Numbness, or loss of feeling, in the arm or hand is also a symptom of this type of nerve damage. In infants, however, it’s difficult for parents or other caregivers to assess whether this is present.

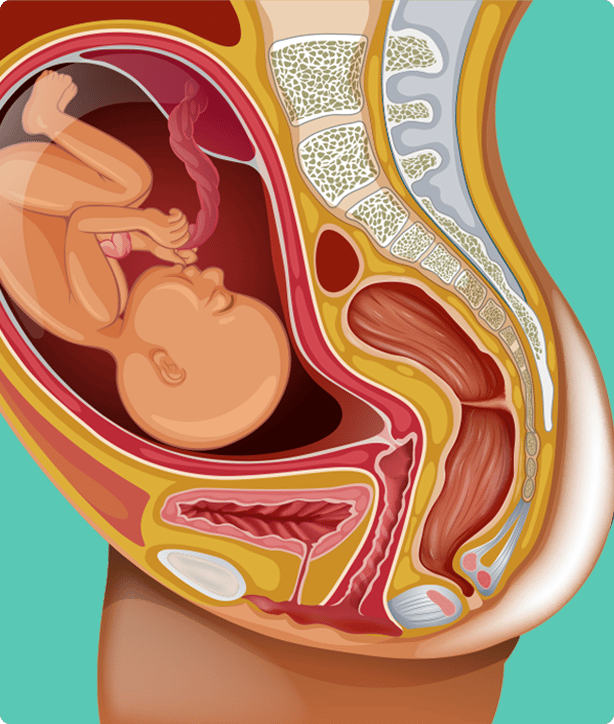
How do brachial plexus injuries occur at birth?
Many factors can increase the chances of a brachial plexus injury at birth. A baby’s brachial plexus is vulnerable during birth, especially the nerves in the shoulder. The severity of the injury can vary, and early diagnosis and treatment are important for positive long-term results.
The existence of these conditions or delivery characteristics can cause injury at birth:
- Baby’s large shoulders gets caught when passing through the birth canal
- Mother has diabetes
- Infant’s shoulders stretched in a head-first birth
- Difficulty getting shoulders to emerge after the head is already out
- Pressure on infant’s raised arms during a feet-first (breech) delivery
- Prolonged, difficult labor
- Pulling of the head and neck sideways as shoulders move through the birth canal
- Twins or multiple pregnancies
- Prior infant delivery with a brachial plexus injury
- Vacuum or forceps improperly utilized can cause excessive pulling that injures the nerves
- Premature birth where underdeveloped nerves and muscles are vulnerable to overstretching
How are brachial plexus injuries diagnosed?
If you are worried that your baby may have a brachial plexus injury, consult with your pediatrician. In diagnosing this birth injury, a physician will examine the baby’s hand and arm and test for functionality and sensation.
If problems persist beyond six weeks, your child will likely be referred for treatment by one or more specialists. Neurologists, neurosurgeons, orthopedic surgeons, physical medicine and rehabilitation doctors, physical therapists, and occupational therapists can all be involved in caring for children with brachial plexus injuries.
Often a doctor will leverage diagnostic tools and procedures to make a diagnosis. A doctor may take an x-ray of the neck and shoulder region to see if there are any fractures or injuries to the dense tissue around the brachial plexus. Magnetic Resonance Imaging (MRI) can also reveal nerve injuries. Nerve conduction studies or electromyograms can help evaluate nerve function and electrical activity as well. However, MRIs and nerve conduction studies are not as reliable for babies as they are for adults.
Sometimes an MRI doesn’t provide a definitive diagnosis. In this case, a doctor may request a test called computerized tomography myelography, more commonly known as a CT scan.
Treatment Options for Brachial Plexus Injuries
If you do receive a positive diagnosis of a brachial plexus injury for your child, don’t despair. First, some injuries will heal by themselves. If your doctor says treatment is necessary for recovery, there are a number of different treatments available depending on the severity of the injury.
It’s important to be realistic about the timeline for recovery from a brachial plexus injury. Nerves can heal slowly, so it may take months or years to see the full results of treatment. Bear in mind that more serious injuries typically require surgery.
Observation
Many brachial plexus injuries heal without medical intervention. In many cases, your child’s doctor will simply observe and monitor the baby’s progress with routine exams. Typically, any spontaneous recovery or improvement happens in the first few months. If your child still has significant symptoms at this point, then medical interventions may be warranted.
Physical Therapy
A physical therapist will recommend an exercise program to help restore your child’s arm and hand function. The therapy will also aim at improving range of motion and reducing muscle and joint stiffness.
Occupational Therapy
If a child has suffered severe muscle weakness, numbness, or pain, occupational therapy will be part of their recovery. Parents are often trained to help the child with movements that will keep the joints and muscles fit for normal daily use.
Surgery
When a baby continues to experience problems from a brachial plexus injury after 3-6 months, your doctor will likely explore surgical options with you. The best chances for a good surgical outcome happen when your child has the surgery between their 4th and 9th month of life. Waiting longer can reduce the potential improvements that surgery can bring.
Your surgeon and doctor will help you determine which type of nerve surgery will help repair or reconstruct your child’s damaged nerves. Surgical options that may be considered include:
- Nerve repair: In this surgery, the doctor reconnects a nerve torn during birth.
- Nerve transfer: A surgeon redirects less important nerves in the arm or chest to perform the functions of the nerve compromised during delivery.
- Nerve graft: The surgical team inserts a healthy nerve from elsewhere in the body to reconnect two ends of a torn or separated brachial nerve.
- Tendon or muscle transfer: A surgeon disconnects a tendon from an injury site and re-attaches it to a healthy muscle to improve damaged or weak muscle function. This surgery is usually done after year one but before adulthood.
- Neurolysis: This surgery can improve nerve function by removing scar tissue from the injury.
- Osteotomy: To improve the function of the upper arm, for example, a surgeon may cut and reorient bones to help the muscle regain strength and heal.
- Capsulorrhaphy: If a child’s shoulder joint is unstable or dislocated during birth, a surgeon will put the humeral head back in the joint and tighten any loose tissue around the joint.
- Free muscle transfers: When healthy local muscles in the arm or hand are not available to replace non-functioning muscles, a surgeon will harvest and transfer leg muscle to substitute for the damaged muscle. This surgery is quite complicated.
Outlook for Babies with Brachial Plexus Injuries
Outcomes and long-term effects of brachial plexus birth injuries vary depending on many factors, including injury severity, timely diagnosis, and the efficacy of employed treatments and surgeries. Many babies heal from these injuries on their own or with modest treatment regimes. However, without proper treatment, babies with severe nerve damage can suffer lifelong disabilities and/or chronic pain. Loss of the use of a hand or arm or use limitations can occur, along with a lack of sensation that poses risks for burns, cuts, or other skin injuries. These repercussions can affect daily tasks where the shoulder, arm, and wrist play a role.
One of the more severe outcomes of brachial plexus injuries can be Horner’s syndrome. This condition occurs as a result of damage to certain nerves of the sympathetic nervous system, which originate in the upper back and help to control functions like pupil size and sweating.
Written by:
Birth Injury Center Team
The Birth Injury Center aims to create informational web content and guides to help women and their families seeking support and guidance for birth injuries caused by medical negligence. All of the content published across The Birth Injury Center website has been thoroughly investigated and approved by medical expert Natalie Speer, RNC-OB, Attorney Ryan Mahoney.


